A combination of nanotechnology, chemotherapy and a monoclonal antibody could treat glioblastoma
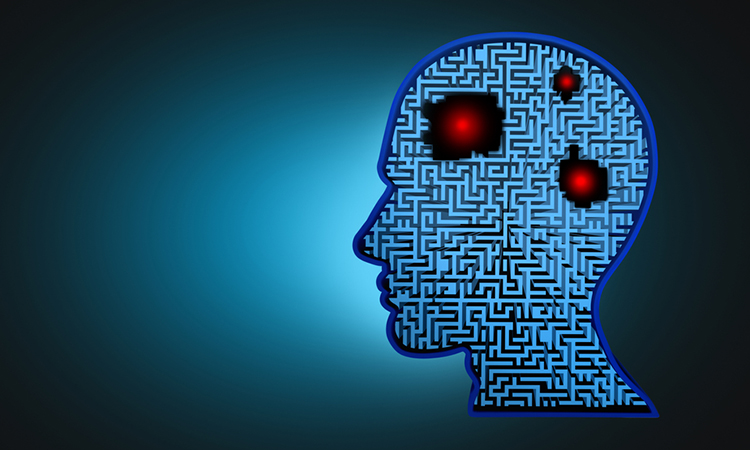
For the first time, researchers have tested a molecule that combines three distinct technologies against glioblastoma, the most aggressive type of brain cancer.
A drug carrier that can reach the brain, bind to glioblastoma multiforme, and release a chemotherapeutic agent has been tested for the first time by researchers from São Paulo State University’s School of Pharmaceutical Sciences in Araraquara (FCFAr-UNESP), Brazil. The study, which was recently published in the International Journal of Pharmaceutics, showed that a combination of nanotechnology, chemotherapy and a monoclonal antibody could treat glioblastoma was effective in both isolated cells and animal models.
Glioblastoma is the most aggressive type of brain tumour. Even after surgery, radiation therapy and conventional chemotherapy, patient survival averages about 14 months. One of the reasons is angiogenesis, a process whereby the tumour quickly creates its own blood vessels to develop.
Another difficulty around this type of tumour is that the blood-brain barrier prevents drugs from reaching the tumour. To navigate around this issue, the researchers combined docetaxel, a powerful chemotherapy drug, with a nanostructured lipid carrier designed to cross the blood-brain barrier. The formulation was developed in such a way that the substances were combined in a stable manner.
The researchers also coupled the carrier to bevacizumab, a monoclonal antibody developed against vascular endothelial growth factor (VEGF) and approved for other uses. The goal was to create a formulation capable of penetrating the brain and releasing a chemotherapy drug to destroy the tumour.
Having created the nanostructured lipid carrier with docetaxel and bevacizumab, the researchers set out to make sure it met certain basic criteria. Laboratory tests showed its size to be 128 nanometres, small enough to overcome the blood-brain barrier. In addition, docetaxel entrapment was 90 percent and bevacizumab coupling efficiency was 62 percent.
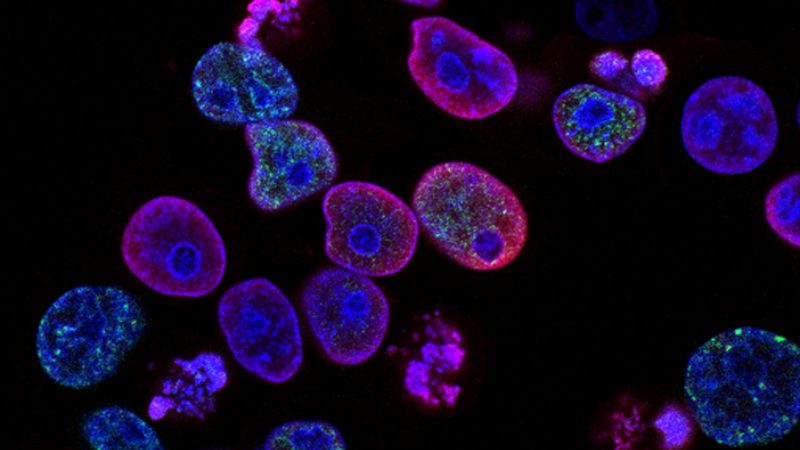
The next step was an assessment of the compound’s effects on two glioblastoma cell lines and healthy cells. The nanocarrier eliminated five times more cancer cells than docetaxel on its own without affecting healthy cells. It was particularly effective against U87MG, a glioblastoma cell that overexpresses VEGF, but less so against A172, which expresses relatively little VEGF.
The researchers also found that the potential medication was able to enter cancer cells and release docetaxel continuously for about 84 hours, suggesting prolonged availability of the chemotherapy drug in the organism.
The rats were inoculated with glioma cells (glioma is a type of cancer similar to glioblastoma). Five days later they were divided into six groups: treatment with placebo; docetaxel alone; nanocarrier alone, without bevacizumab or docetaxel; nanocarrier and bevacizumab, without docetaxel; nanocarrier and docetaxel, without bevacizumab; nanocarrier with docetaxel and bevacizumab.
After 15 days, the first four groups were found not to have benefited from the treatment. In the fifth group (nanocarrier with docetaxel) and sixth group (nanocarrier with docetaxel and bevacizumab), tumour volume was reduced by 40 percent and 70 percent respectively.
“We need to conduct more studies using isolated cells and animals. If the results against glioblastoma multiforme remain good, we could try to find partners for clinical trials with human volunteers,” concluded Professor Marlus Chorili, a principal investigator of the study, “We can use different combinations with other monoclonal antibodies and chemotherapy drugs against other types of cancer. Many more years will undoubtedly be required to complete this research.”