Technion researchers offer ‘Hope’ for treating diabetes, minus the painful jabs
(March 15, 2023, JNS Wire) Technion–Israel Institute of Technology Professor Shady Farah knows all too well the hardships diabetes patients suffer. As a boy of 12, he had to give his grandmother insulin injections daily. “It’s tough,” he said. “You love her and care about her, and it causes pain.”
He recalled she would often tell him, “ ‘Shady, maybe one day you can help find a cure for this.’ ”
Neubauer Assistant Professor Farah took her words to heart. He and assistant professor Joshua Doloff of Johns Hopkins University recently received a $700,000 grant from the Juvenile Diabetes Research Foundation (JDRF) to advance their efficient, pain-free solution for people suffering from Type 1 or “juvenile” diabetes, a chronic condition in which the pancreas produces little or no insulin by itself.
If successful, the new technology, dubbed “Hope,” could do away with painful insulin injections, changing the face of diabetes for an estimated 8.4 million people living with diabetes worldwide.
Diabetes patients have a variety of options to manage the disease, but all come with difficult challenges. In the traditional approach, patients prick their fingers to obtain a droplet of blood, measure their glucose level, inject themselves accordingly and prick again to ensure they got it right. This method is the most accurate, but patients usually need to test themselves several times a day.
Alternatively, patients can opt to wear a Continuous Glucose Monitoring (CGM) system, consisting of a sensor inserted under the skin on their belly or arm, an insulin pump and a transmitter that alerts the wearer’s smartphone when they need to release insulin. But CGMs are not always accurate, and the sensor can cause scar tissue if left in too long.
There is a third treatment option that appears promising: transplanting “islets” or clusters of healthy donor pancreatic cells that sense the patient’s glucose level, produce insulin and release it into the patient. But like all transplants, these artificial biological pancreases run up against the immune system, which is trained to recognize and attack foreign objects. Patients must continuously be on immunosuppressant drugs to prevent the body from sealing off the islets behind a wall of fibrotic scar tissue, killing the transplant. Scientists have improved the process by encapsulating the islets in jelly-like hydrogels that provide nutrients, oxygen and some protection from the immune system, but not enough.
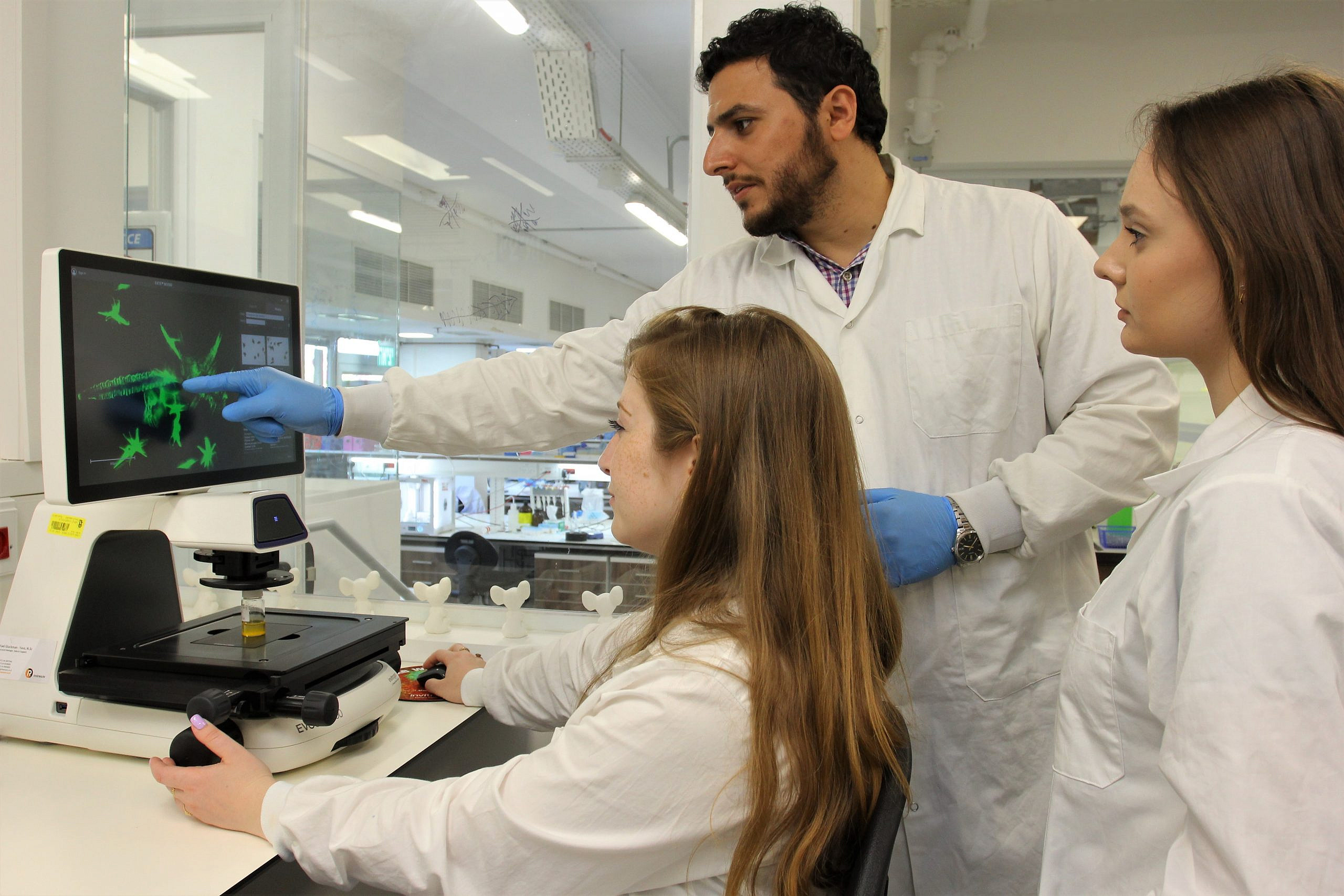
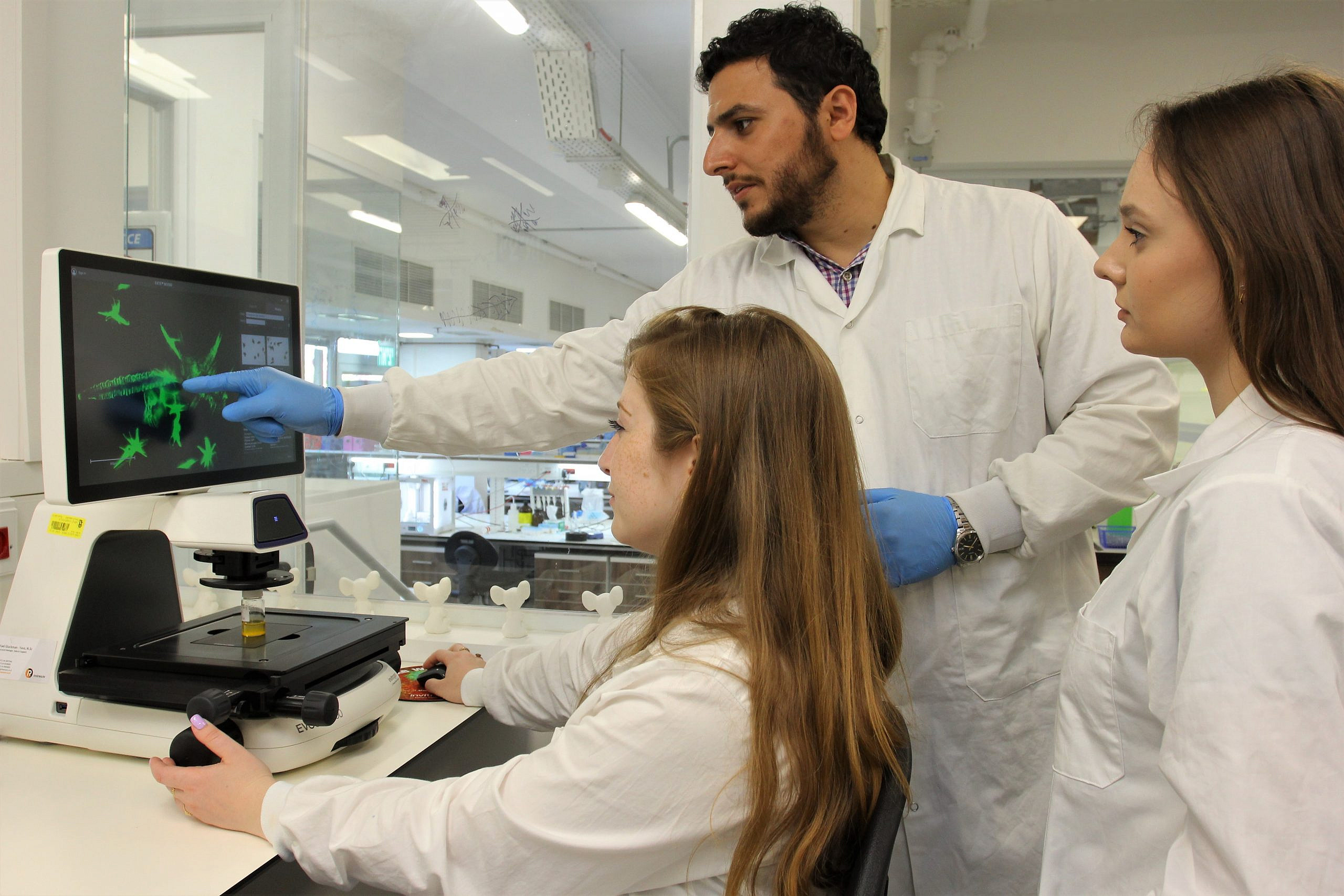
Technion–Israel Institute of Technology Professor Shady Farah with a member of his research team in Haifa. Israel. Credit: Courtesy of the Technion Israel-Institute of Technology.
‘I want to make a difference’
That’s where professors Farah and Doloff come in.
While working together at the Koch Institute at the Massachusetts Institute of Technology and the Boston Children’s Hospital/Harvard Medical School, the then-postdoctoral fellows came up with a novel way to avert fibrosis and unwanted immune responses in pancreatic transplants, allowing the islets to do their job. They developed crystallized drugs that target the key players of immune system rejection and incorporated them into the hydrogels holding the insulin-producing islets. As crystals take a long time to dissolve, the drugs are secreted slowly, selectively dampening the immune response in the area immediately surrounding the hydrogel while leaving the rest of the immune system untouched.
The new JDRF grant will allow Farah and Doloff—and their teams in the Wolfson Department of Chemical Engineering and the Russell Berrie Nanotechnology Institute at the Technion and Johns Hopkins’ Whiting School of Engineering’s Department of Biomedical Engineering, respectively—to develop a newer, more advanced version of these crystals, which the Stedelijk Museum Breda in the Netherlands included in their exhibit “True Beauty” of the most beautiful images in 21st-century science. Farah and Doloff’s next-generation crystals would protect more complicated transplants, such as grafts from animals to humans and stem cells that could be differentiated into specialized pancreatic cells, providing patients with a larger pool of tissue for transplants.
They call their crystals “Hope” because “it might help us treat many conditions in the future, not just diabetes,” said Farah. The advanced crystals could be applied to other implantable medical devices such as pacemakers, stents or sensors. Already, the crystals have shown promise in preclinical trials, curing diabetes in mice for 1.3 years without creating fibrosis or a need for insulin injections. If all goes well, Farah believes the technology could be commercialized in five to 10 years.
Born and raised in the small Galilean village of Kfar Yasif, Farah; his wife, Dr. Amani Jahjaa-Farah, a pediatric resident at Rambam Healthcare Campus in Haifa; their two children, Emily and George; and his extended family trace their heritage to the ancient and first sect of Christians in the days of Jesus. His village has turned out some of the most highly educated Arab doctors and academics in Israel, and Farah is fast joining those ranks with his work on the immune system and other areas.
He earned his Ph.D. in Medicinal Chemistry from the Hebrew University of Jerusalem, conducted his postdoctoral studies abroad, and then joined the faculty at the Technion in 2019. There, he founded the Laboratory for Advanced Functional/Medicinal Polymers & Smart Drug Delivery Technologies—a multidisciplinary group of researchers that includes chemists, chemical and biomedical engineers, materials scientists, pharmacists and pharmaceutical
engineers, physicians and even a dentist. Among the group’s achievements, they developed an effective technology, a long-lasting disinfectant to target the coronavirus on surfaces.
Doloff received his bachelor’s degree from the University of Pennsylvania and his graduate degrees from Boston University. In addition to his post in Johns Hopkins’ Department of Biomedical Engineering, he is a member of the Translational Tissue Engineering Center at Johns Hopkins University School of Medicine. His lab is interested in systems biology with an emphasis on engineering improved therapies in the fields of cancer, autoimmunity, transplantation medicine, including Type 1 diabetes and ophthalmology.
“I’ve seen many people with diabetes, and I want to make a difference,” said Farah. “With this grant, I hope we can develop technologies to help patients with Type 1 diabetes because they really are suffering and deserve a more convenient lifestyle.”
Jennifer Frey is a writer and editor at the American Technion Society.



